 Estimated reading time: 2 minutes
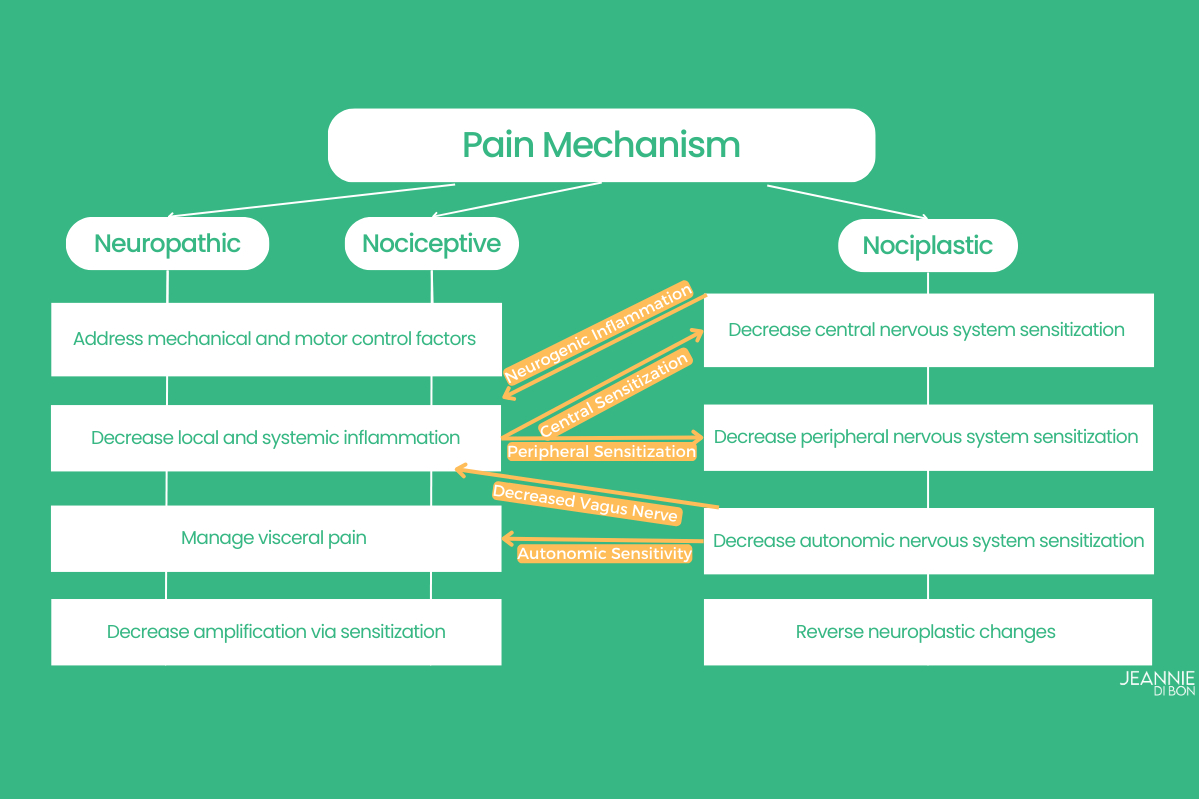
Estimated reading time: 2 minutesOur previous post described the 3 types of pain: Neuropathic, Nociceptive, and Nociplastic. Knowing which type(s) of pain you have can help you manage pain more effectively. Think of it like taking your car to the mechanic – if they replace the air filter when you have a flat tire, it won’t fix the car. You have to address the correct problem. Similarly, different types of pain are managed differently.
Reminder: People with HSD/hEDS may have any or all three types of pain, and it may change day by day.
Issues with the Tissues
Nociceptive and neuropathic pain are caused by mechanical factors, inflammation, or disease affecting the tissues. The previous diagram shows several ways to address “Issues with the Tissues.”
Instability
First, address the mechanical factors stressing the tissues. Mechanical pain is often caused by joint instability. This occurs when muscles and nerves controlling muscles are not properly controlling joint movement. It isn’t the hypermobility that is causing the pain but the instability.
Instability is addressed by:
- Improving proprioception and motor control
- Activating stability muscles
- Learning to relax power muscles that might be overactive (guarding or bracing)
Muscles often go into spasm because they are trying to improve stability, but the muscles in spasm are usually not the right muscles to provide stability. Activating the right muscles can allow the muscles in spasm to relax.
Managing mechanical factors affecting nerves often involves addressing areas where nerves are compressed or stretched. For example: Nerves traveling from the neck into the arm may be compressed by scalene muscles in the neck. Scalenes are often overactive when people breathe into their chest instead of their belly. While they can help with breath, scalenes are not designed to be active 24/7. When these nerves are compressed Thoracic Outlet Syndrome can occur.
This is a mechanical nerve problem that can be fixed with appropriate posture, body mechanics, and exercise.
Inflammation
Tissues and nerves can both be affected by inflammation. Inflammation due to local tissue damage can be managed with local strategies such as ice or topical anti-inflammatory rubs. But systemic inflammation, such as that caused by Mast Cell Activation Disorder, needs to be managed systemically by calming the immune system or with anti-inflammatory or antihistamine medications.
The vagus nerve is known to decrease inflammation throughout the body, so techniques to activate the vagus nerve can decrease systemic inflammation. Neurogenic inflammation is caused by a sensitive nervous system, so the sensitive central nervous system needs to be addressed.

This diagram also shows three ways in which we can manage “Issues with the Tissues”: Prevent problems, fix problems, and soothe pain. For example, good posture and body mechanics can prevent problems such as headaches caused by trigger points in the neck muscles. Strengthening muscles around the shoulder can fix instability. Strategies like ice, heat, transcutaneous electroneural stimulation (TENS), and topical medications can soothe the pain.
The Zebra Club can help with these! Classes focus on learning body mechanics and posture and finding stability and strength.
See Managing Nociplastic Pain with Dr. Leslie Russek to learn more.
September is Pain Awareness Month and I am honored to have Dr. Leslie Russek join me to discuss pain in hypermobility. Dr. Russek PT, DPT, PhD, OCS is not only my colleague and research partner, but also the scientific advisor to The Zebra Club where she regularly shares her vast knowledge of hypermobility spectrum disorders. Find more information including generous free resources here.
No Comments