 Estimated reading time: 6 minutes
Estimated reading time: 6 minutesNeck pain is also commonly accompanied by headaches (2). In a recent study of people diagnosed with a hypermobility condition, 66% reported headache, neck pain, neck instability or clicking, facial pain, or a combination of these (3). While it is hard to talk about one without the other, we will focus on the neck in this post.
Reduced joint stability and muscle strength, when combined with hypermobility, can play a significant role in the development of neck pain. This is a complex topic as the neck doesn’t exist in isolation and can be impacted by the muscles and joints both above and below.
Factors that may influence neck pain in hypermobility
- TMJ
- Temporomandibular joint (TMJ) hypermobility is associated with neck myofascial pain (4). Headache and neck pain were the most frequently reported co-occuring conditions reported by a group of people with EDS and TMJ pain (5). TMJ disorders are also associated with craniocervical instability (6). While it can be hard, finding a hypermobility aware jaw pain specialist can be beneficial. Anecdotally, orofacial myofunctional therapy may also help.
- Altered proprioception of the neck
- In a group of people diagnosed with generalized joint hypermobility (based on a Beighton score of >4/9), non-specific neck pain was associated with a decreased ability to position the neck back to a previously held position. This was attributed to lack of proprioception of the neck. This was significantly different than asymptomatic hypermobile individuals (1)
- Forward head posture
- With every inch forward it is estimated that an extra ten pounds is added that the upper back and neck must support (7). The deep and rear muscles of the neck work together to protect the cervical spine (first 7 vertebrae) from the forces of gravity. This allows the neck to maintain stability during daily activities. It is thought that when the muscle function is impaired, there is a disruption in the balance between the muscles in the front and back of the neck will result in loss of the natural curve of the neck (cervical lordosis). This could contribute to neck issues (1)
Craniocervical/Upper Cervical instability is common in hypermobility
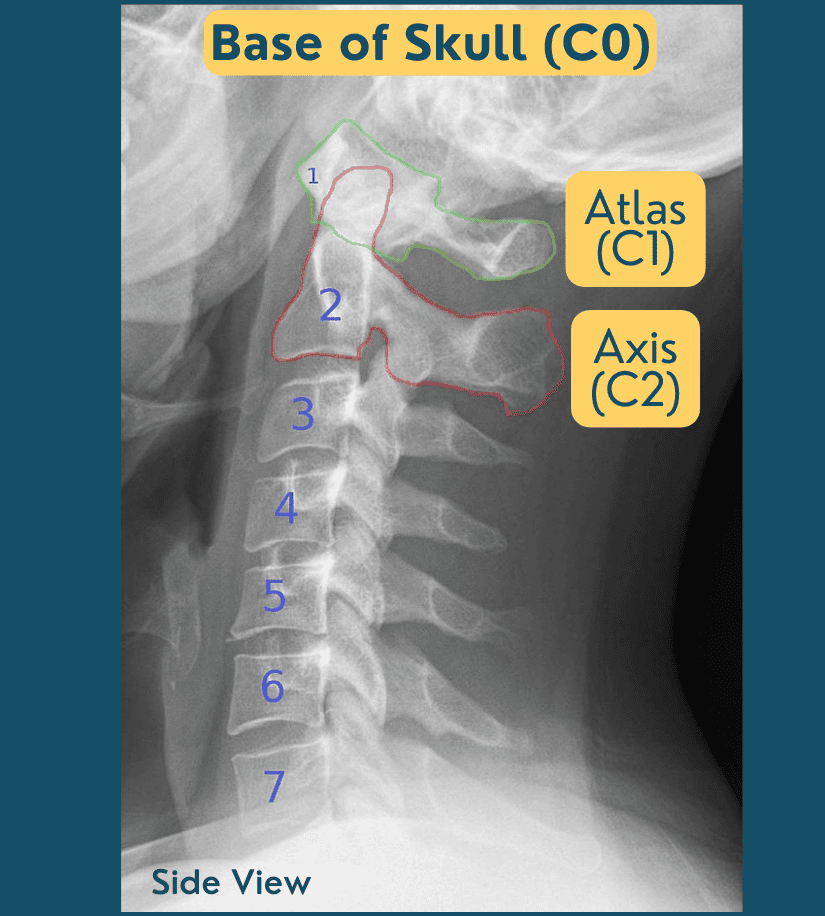
Craniocervical instability is something I get asked about frequently. Upper cervical spine hypermobility can cause headaches directly in response to certain neck movements like lateral rotation and flexion (4). Upper cervical instability (UCI) is instability in the joint between the atlas (C1) and occiput (C0, base of skull). This is called Atlanto-occipital/craniocervical instability (AOI or CCI). It may also involve the joint between the atlas (C1) and the axis (C2). This is called atlantoaxial instability (AAI).
Mild UCI is relatively common, affecting 52-66% of people with hEDS/HSD. Severe UCI is uncommon affecting only 5% of this population. UCI is also likely underdiagnosed (8).
Symptoms of UCI Include headaches, neck or facial pain, dizziness, vertigo, nausea, numbness/tingling, shortness of breath, difficulty speaking, vision changes (blurred, tunnel vision, auras), hearing changes, difficulty swallowing, choking, sleep apnea, memory deficits, pre-syncopal episodes (feeling like you’re going to faint) (8).
The Zebra Club’s Scientific Advisor Dr. Leslie Russek and an international team of physical /physiotherapy clinicians, researchers, and a hypermobility specialist rheumatologist recently published guidelines for physical therapy treatment and assessment of UCI. For a determination of UCI – three criteria must be met:
- Symptoms are consistent with musculoskeletal and/or neurological UCI.
- Symptoms are altered by neck movement or position. For example:
- Symptoms increase with leaning forward or looking down
- Symptoms increase with neck motions like flexing, extending or rotating
- Mechanical irritability with a physical exam
Patients are classified as having low, moderate, or high “irritability.” This is a measure of mechanical irritability. This is based on how severe the condition is, how easily it is flared, and how long it takes for symptoms to calm down after being flared. They also state that high irritability is likely uncommon. Importantly, they point out that this may change from day to day and progress towards lower irritability as patients improve. They stratified their recommendations based on the level of irritability.
Managing hypermobility and CCI/UCI in the neck
Here are some of the recommended interventions that were deemed safe for all levels of irritability (8), all of which I find helpful in my clinical practice and in The Zebra Club app.
- General education about hEDS/HSD and UCI
- Education in posture and body mechanics
- Sitting, standing, and sleep posture, positioning, and body support
- Body awareness and mindfulness in various positions (sitting, standing, lying down)
- Functional training for posture and joint protection for essential daily activities (like bathing, brushing hair, washing hair, etc)
- Relaxation and autonomic nervous system balancing (not requiring neck movement)
- Breathing (diaphragmatic or slow breathing)
- Education in pain neuroscience
- Self-care “toolbox”
- pain management strategies like TENS, topicals, heating pads, relaxation, etc.
I would add:
- Avoid stretching the neck – this can cause instability and pain
- Listen to your body – if an exercise causes pain, discontinue it.
- Little and often – consistency is key to building stability.
Daily challenges and impact on life
Neck instability can pose challenges to daily activities – both physical and overall quality of life.
- Pain and discomfort can limit activities and routine tasks can become difficult. Many patients report things like visiting the hairdresser or the dentist chair are challenging.
- The use of ergonomic tools and furniture can help. Be mindful of how you use your phone or read a book. Some find glasses like these can be helpful when the neck is flaring.
- You’ve probably heard of text neck, this can be a major contributor to neck pain, and something we can address with practice.
- Driving the car and needing to rotate the head can mean driving is avoided. If you are a passenger in a car, it is worth looking into a cervical neck brace to support the neck over bumps and turns.
- Fatigue – overcompensating for instability can lead to increased fatigue.
- Pacing – prioritize rest and pacing
- Sleep disturbances – neck pain can disrupt sleep and lead to a vicious cycle of pain and fatigue. Consider your pillows and the type of mattress or support you might need.
- For activities like cleaning, cooking, and carrying groceries, try to use tools that minimize strain. You can get long-handled dusters for example. An OT may be able to work with you to find adaptations for your situation. And definitely, ask for help.
- Clothing choices – when your neck pain is in a flare, choose clothing items that are easy to take on and off. Maybe a shirt over a pullover or sweatshirt.
Essential exercises for neck hypermobility
- Proprioception exercises are key. As mentioned above, the ability to position the cervical joint and maintain muscle endurance (flexor and extensor holding capacities) were impaired in hypermobile patients with neck pain (1). Many therapists recommend the use of a laser light to give biofeedback on this positioning.
- A common mistake often made with the hypermobile neck is to jump in with neck exercises. When I work with neck instability including CCI and AAI, I never start with the neck. The head and neck need to be supported from below – all the way down to the feet.
- Chin tucks are often prescribed, but I would heed caution with these with irritable necks. If not performed correctly, they can lead to shearing of the cervical vertebrae and can cause neurological issues. These are not recommended for people with high levels of UCI irritability (8).
- Mindfulness and deep breathing exercises can help calm the nervous system and reduce stress and worry about neck pain. It can also be helpful to speak to a trained therapist in anxiety management.
- Neck isometrics also need to be approached with caution – they are not suitable for everyone and can cause neurological symptoms.
- Exercise can be beneficial but working with someone who is aware of EDS is essential. Whole-body integration is key for neck instability.
Living with neck instability requires a multifaceted approach that includes physical, emotional, and lifestyle adjustments. Working with an EDS-aware therapist like movement specialists, physical therapists and occupational therapists can be really helpful in minimizing the impact it has on daily life.
Here is a video including education and a movement practice I designed for neck pain.
Literature Review and Research by Catherine Nation, MSc, PhD
Works Cited
- Reddy et al (2022) Comparison and correlation of cervical proprioception and muscle endurance in general joint hypermobility participants with and without non-specific neck pain—a cross-sectional study. Peerj.
- Chopra et al (2017) Pain Management in the Ehlers-Danlos Syndromes. American Hournal of Medical Genetics Part C (Seminars in Medical Genetics).
- Malhotra et al (2020) Headaches in hypermobility syndromes: A pain in the neck. American Journal of Medical Genetics, Part A.
- Castori et al (2017) Connective Tissue, Ehlers-Danlos Syndrome(s), and Head and Cervical Pain. American Journal of Medical Genetics Part C (Seminars in Medical Genetics).
- Di Giacomo et al (2018) Evaluation of Temporomandibular Disorders and Comorbidities inPatients with Ehler‑–Danlos: Clinical and Digital Findings. Journal of International Society of Preventive and Community Dentistry.
- Mitakades and Tinkle (2017). Oral and Mandibular Manifestations in the Ehlers-Danlos Syndromes. American Hournal of Medical Genetics Part C (Seminars in Medical Genetics).
- Raykar et al (2018) Effect of forward head posture on static and dynamic balance. World Journal of Pharmaceutical Research.
- Russek et al (2023) Presentation and physical therapy management of upper cervical instability in patients with symptomatic generalized joint hypermobility: International expert consensus recommendations. Frontiers in Medicine.
4 Comments
Alison K - 6th April 2022
Will you be doing another one of these? Thanks!
Jeannie Di Bon - 7th April 2022
Yes, I just did one with EDS Awareness. You can watch the session on their website at http://www.chronicpainpartners.com. Hope it is useful.
Jill BONHAM - 13th May 2021
Been having migraines for decades and finally worked out that I’m hypermobile and this is causing me to wake up nightly with migraines which nothing has been able to fix… Go to an osteopath that’s the best treatment but I think I need to do something about it as doctors and even neurologist just seem not interested
Jeannie Di Bon - 17th May 2021
Thank you for your comment. Hope you find a solution that works soon.