
Estimated reading time: 11 minutesI always start at the feet.
The foot needs to be stable and mobile at the same time for good foot mechanics. It is super important to understand the relationship between the foot and the rest of the body.
The foot will impact the knee, hip, lower back, and upwards from there. Even asymptomatic hypermobile feet and ankles can contribute to pain all the way up the body (1).
There are two major foot movements that we need to be able to do for healthy foot mechanics – pronation and supination.
Pronation sees a flattening of the foot and internal rotation of bones. Supination sees a lifting of the arches and external rotation of bones.
Research shows that people with joint hypermobility syndrome can have multiple alterations in walking patterns, including reduced walking speed, altered stepping patterns, and stiffened joint movement when walking (probably an effort to avoid pain or protect the joint) (2).
This points to a need for gait training and learning how to effectively move our feet.
Importantly, the muscles in the foot can be deconditioned just like any other muscle in the body. The good news is we can learn how to work these muscles to support balance and posture, and rehab our bodies from the foot up. We need to find a way to give our feet structure and support whilst maintaining foot mobility.
Key Takeaways
Hypermobile feet affect the entire kinetic chain, causing pain in knees, hips, and back. Movement therapy addresses this through four key areas: improving mobility, developing stability without guarding, calming the nervous system, and strengthening to support the whole body. Balance training shows exceptional results—even better outcomes than in non-hypermobile populations. Understanding the difference between collapsed feet (structural issue) and pronated feet (healthy movement) guides effective treatment. Collaborate with EDS-aware podiatrists when orthotics are needed.
Why foot mechanics matter in hypermobility
The foot needs to be both stable and mobile simultaneously for proper function. In hypermobility, this balance can be disrupted. Ligament laxity allows excessive movement while compromising stability.
Even asymptomatic hypermobile feet can cause pain throughout the kinetic chain, affecting knees, hips, and the lower back, because altered foot mechanics change your entire posture and gait pattern.”
“When the foot hits the ground, a whole body reaction occurs.”
The feet are so important.
Ideally, for healthy foot positioning, we want to aim to stand on a tripod or a neutral foot. The tripod is made of the heel bone, big toe pad, and little toe pad. This makes up the support structure of your foot. In a neutral position, the three points will be in contact with the ground.
When we walk, we push off the big toe bone or first metatarsal. It gives us the power to push off and activate the whole posterior chain to move through the step.
We need to pronate when we walk. When we step into the foot, we lengthen and widen to allow the foot to move and adapt to the impact of the ground. If we didn’t, there would be too much stress going through the joints.
So many of us have issues around many of the joints and foot structures that can lead to altered gait patterns, altered posture with standing, and pain.
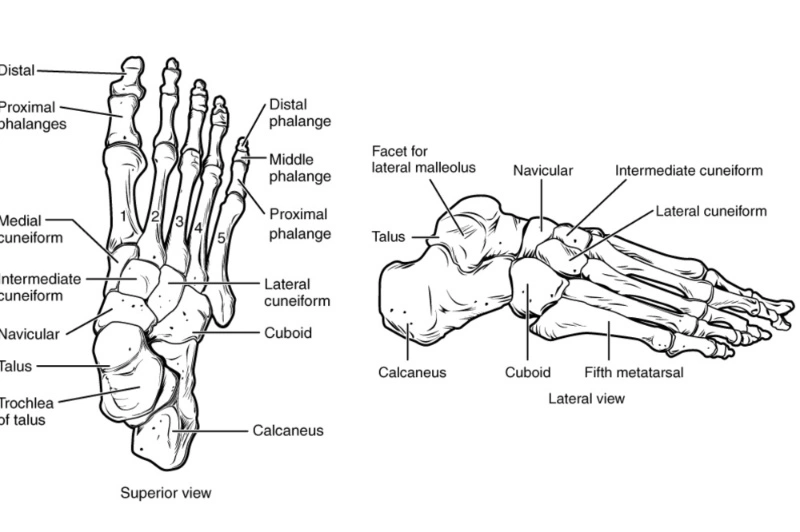
Anatomy: 26 Bones, 33 Joints, and How Hypermobility Affects Movement
The foot is made of 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments all working together to support weight, absorb impact, and propel the body forward. Feet are made for movement!
The bones of the feet are:
- Talus – the bone on top of the foot that forms a joint with the two bones of the lower leg, the tibia and fibula.
- Calcaneus – the largest bone of the foot, which lies beneath the talus to form the heel bone.
- Tarsals – five irregularly shaped bones of the midfoot that form the foot’s arch. The tarsal bones are the cuboid, navicular, and medial, intermediate, and lateral cuneiforms.
- Metatarsals – five bones (labeled one through five, starting with the big toe) that make up the forefoot.
- Phalanges (singular: phalanx) – the 14 bones that make up the toes. The big toe consists of two phalanges – the distal and proximal. The other toes have three.
- Sesamoids – two small, pea-shaped bones that lie beneath the head of the first metatarsal in the ball of the foot.
What problems are common in hypermobility?
Hypermobile feet commonly experience ankle instability with frequent rolling or sprains, plantar fasciitis with heel pain, and either flat feet (collapsed arches) or paradoxically high arches.
These conditions occur more frequently and severely than in the general population due to ligament laxity affecting the foot’s structural support.
Ankle instability and chronic sprains
Ankle instability is one of the most common complaints in hypermobility, with frequent rolling, chronic sprains, and persistent pain. Loose ligaments cannot adequately stabilize the ankle joint, leading to higher re-injury risk and longer recovery times. The good news: research shows balance training is particularly effective for ankle instability in hypermobile people.
One research group set out to assess balance training as a treatment for chronic ankle instability. They compared their balance training protocol in a group of people with chronic ankle instability (based on MRI) and split them into two groups – one considered to have generalized joint hypermobility, which they categorized as having a Beighton score greater than or equal to 4.
They found that patients with generalized joint hypermobility had even better outcomes with balance training than the less hypermobile group. They found an improvement in sprain recurrence, balance control, and muscle strength (3).
Balance is a key tenet in my Integral Movement Method; I have a whole chapter devoted to the foot and balance in my new book, The Integral Movement Method for Hypermobility Management. I believe balance is essential for everyday life, and love seeing this improve in my clients when we work together.
Plantar fasciitis and heel pain
This is a painful condition occurring at the bottom of the feet, which is often worse in the morning or after long periods of rest. This is a painful foot condition I often see in my clients.
The plantar fascia is a thick band of connective tissue that provides support to the arch and helps provide structure for propulsion and energy for stepping (4).
This is thought to be due to an issue with where the plantar fascia connects with the calcaneus (heel bone)(5).
Here is a short video on how to manage this condition.
Do people with EDS have flat feet or high arches
Many people with hypermobility have flat feet (pes planus) with collapsed arches, but not everyone—some actually have high arches (pes cavus). Both conditions can cause problems.
An important distinction: collapsed and pronated feet are not the same thing.
Pronation is a normal, healthy three-dimensional movement where the foot flattens and rotates inward to absorb impact during walking. Every healthy foot pronates as part of natural gait mechanics. Collapsed feet, however, occur when ligament laxity allows the foot structures to slide inward and flatten excessively under gravitational pull, even when standing still.
Hypermobile feet often struggle with both: they collapse when standing, but also need to learn how to pronate properly during movement.
In a hypermobile flat foot, there is going to be a tendency for the bones to rotate inwards, causing the ‘knock-kneed’ look or X legs. The thigh bones then roll inwards, which tends to lead to an anterior tilt of the pelvis.
You can work at trying to fix the anterior tilt, but unless you also look at the mechanics of the foot upwards, it probably won’t be successful. You have got to take a global look at the body. The Letter X on the A to Z of hypermobility looks at this X-leg issue and how to correct it.
Different studies have found both a higher prevalence of flat feet (pes planus)in hypermobility(6) and a higher prevalence of high arches (pes cavus) in hypermobility (7).
I tend to see more flat than high arches, but what is important is that this can be changed and worked on to improve mechanics.

Other conditions commonly seen
Beyond ankle instability, plantar fasciitis, and arch variations, hypermobile feet may experience additional conditions due to altered mechanics, friction from imbalanced movement patterns, and delayed healing:
- Blisters
- If we have imbalances in how we walk and stand, friction can cause blisters
- Bunions
- Or Hallux Valgus is commonly seen in Ehlers-Danlos Syndrome (8)
- Neuroma (nerve tumor or Morton’s neuroma)
- If the metatarsals move too much due to hypermobility, friction on the interdigital nerves can occur which could lead to a neuroma.
- Ingrown toenails
- The nail grows into the toe, usually the big toe.
- Corns and calluses
- Friction and imbalance can cause these to develop. I can always tell a lot about how my clients walk by looking at the calluses on their feet.
- Overuse injuries and strains
- This is very common in hypermobility. Mechanics and gait improvements can help prevent this.
- Heel pain
- Working on developing a tripod can prevent excessive heel pressure and pain.
- Clawed toes
- I was guilty of this. I would claw my toes as a form of stability. The feet are often the last resort when all other stabilisers have failed. It also meant I was very front-body dominant, which I see a lot in my clients.
- Arthritis
- While hypermobility itself doesn’t cause arthritis, it can contribute to joint wear and tear, potentially increasing the risk of developing arthritis over time, especially in weight-bearing joints (Arthritis UK)
- Athletes foot
- A common fungal infection that affects the feet. It can be treated with creams and sprays. The symptoms can cause itchiness, inflammation of the skin, blisters, and stinging. These will all impact our correct walking patterns, so it is important to have these infections looked at as soon as possible.
- Delayed wound healing
- We know that EDS wounds tend to take longer to heal, which will impact proper gait mechanics due to pain.
- Small fiber neuropathy
- This is beginning to be found commonly in people with hEDS (9). This may feel like burning feet or pins and needles.

Why does hypermobility cause foot pain?
Hypermobility causes foot pain through multiple mechanisms: ligament laxity creates joint instability, gravity constantly pulls on already-loose structures, causing collapse, and altered foot mechanics create compensatory strain throughout the kinetic chain.
This means foot pain in hypermobility isn’t just a local problem; it can trigger pain in the knees, hips, lower back, and beyond.
Even asymptomatic hypermobile feet—feet that don’t hurt themselves—can cause pain throughout the entire kinetic chain. When foot mechanics are altered, the body compensates by changing how the knees, hips, pelvis, and spine function, creating a cascade of strain that can result in pain far above the feet.
Some reasons you may be experiencing foot pain with hypermobility:
- Alignment & Posture
- Alignment of the bony structures is key.
- Laxity of joints
- Structure
- Structural issues can lead to conditions like bunions and neuromas.
- Gravity
- This is pulling us down and potentially flattening our feet
- Environment / Job / Home / Stress
- Do I exercise my feet enough? Do I wear shoes all day so they are not moving naturally?
- Spinal / Pelvic Instability
- The feet impact the pelvis and vice versa. If I have a twisted pelvis, that is going to cause more weight in one foot than the other.
- Immobility in other areas
- Proprioception & Motor Control
- Lack of proprioception in the feet has been found in people with EDS (10)
- Check out this video to learn more about proprioception
- Balance
- A super important part of any EDS/HSD training programme is to work on balance. The act of walking is, in fact, a balancing act. My video Letter B for Balance and Breath gives you some simple exercises to try.
- Breathing
- If we more frequently use high-up chest breathing, this can disrupt our balance. We need to get weight down into the feet, but without collapsing into them.
The good news is that there are things we can do to address so many of these issues and improve your pain.

In this class in The Zebra Club called Resolve Feet and Gait Pain, we learn ways to optimize gait patterns to reduce pain from the feet, all the way up the body.
Understanding footwear and orthotics
Proper footwear and custom orthotics provide external structural support that compensates for ligament laxity in hypermobile feet. We also want to work on strengthening the feet in addition to any supports used.
What research shows about custom orthotics
Custom orthotics and proper footwear can go a long way in improving foot pain.
One study assessed the use of custom orthotics in people with EDS and found that wearing custom insoles for 3 months (7 hours a day) led to improvements in foot pain, foot functionality, fatigue(!), and mental-health-related quality of life. This was based on questionnaires filled out by participants the day the orthotics were received and 3 months later (11).
Sophie Roberts and Alan Hakim also state that orthotics help improve proprioception, help with ankle stability and recurrent sprains, and help with issues further up the kinetic chain (knees, hips, back) by changing foot kinematics (or motion of the foot) (1).
The orthotics mentioned in both publications were created by podiatrists who had an awareness of EDS, which is sadly not always our experience.
While research demonstrates significant benefits, **whether you specifically need custom orthotics depends on your individual situation**. Factors include your specific foot structure, symptom severity, activity level, and movement patterns.
Not everyone with hypermobile feet requires orthotics—some people achieve excellent results with strengthening and movement therapy alone. An EDS-aware podiatrist can assess your feet, analyze your gait, and determine if custom orthotics would support your specific needs and movement therapy goals.
Working with an EDS-aware podiatrist
As movement specialists, we work collaboratively with podiatrists who understand hypermobile biomechanics. While we guide movement strategies, strengthening, and gait training, podiatrists bring expertise in assessing foot structure, analyzing gait mechanics, determining orthotic needs, and providing footwear guidance based on your individual biomechanics.
Working with EDS-aware podiatrists like Sophie Roberts can guide you in shoe and orthotic selection, working with your individual patterns and gait. The Zebra Club members can watch a past presentation from Sophie Roberts in the Resources Section of the App (Presentations > Sophie Roberts on Podiatry – September 2023).
Some favorite shoe brands of The Zebra Club members include Hokas, Brooks, and Oofos.

How does movement therapy help?
Movement therapy for hypermobile feet focuses on four key areas: improving pain-free mobility, building stability without bracing or guarding, calming the nervous system to reduce pain sensitization, and strengthening to support both body and mind. ‘
Research shows these movement-based approaches are highly effective for hypermobile individuals, with some interventions working even better than in non-hypermobile populations.
When I address the foot with my clients, these are some of the main things I focus on:
- Mobility
- The ability to start to move pain-free
- Try this: foot mobilization exercises with a spikey ball
- Stability
- Finding stability without guarding or bracing
- Try this: standing on one leg whilst holding on
- Calming of the nervous system
- This can help with pain sensitisation
- Try this: breathing exercises
- Strength
- To support the foot and ankle and subsequently the whole kinetic chain
- Try this: foot strengthening exercises
You can find classes to address each of these aspects in The Zebra Club app
Video: Solutions for Hypermobile Feet
In this video, I dive into all things feet, the issues we face in hypermobility, and how we can address these issues with movement.
FAQ
How does hypermobility affect your feet?
Hypermobility in the feet may lead to ligament laxity, impacting the alignment and structure of the feet. This can impact movement and mechanics and cause pain all the way up the body. The good news is that we can learn how to strengthen the feet to gain structure and stability and maintain mobility.
What is the test for hypermobility in feet?
There are several ways to test for hypermobility in the feet. We need to assess how easily the joints move beyond a typical range of motion. Tests could include dorsiflexion of the little toe, the navicular drop test, the toe flexibility test, midfoot and rear foot mobility test, ankle dorsiflexion test.
Is walking bad for hypermobility?
Walking can be a great form of exercise for people with hypermobility. If you are experiencing pain while walking, you may need to address foot strength and gait mechanics. Wearing supportive shoes and custom orthotics can also be helpful in the meantime. The good news is there are things we can do to improve your walking and reduce pain.
Can hypermobile feet cause knee, hip, and back pain?
Even asymptomatic hypermobile feet—feet that don’t hurt themselves—can cause pain all the way up the body. When foot mechanics are altered, the body compensates by changing how the knees, hips, pelvis, and spine function, creating a cascade of strain. You have got to take a global look at the body. Improving foot mechanics can help reduce pain throughout the entire kinetic chain.
What’s the difference between collapsed feet and pronated feet in hypermobility?
Pronation is a normal, healthy movement where the foot flattens and rotates inward to absorb impact during walking—every healthy foot pronates. Collapsed feet, however, occur when ligament laxity allows the foot structures to slide inward and flatten excessively under gravitational pull, even when standing still. Hypermobile feet often struggle with both: they collapse when standing, but also need to learn how to pronate properly during movement.
Why is balance training so effective for hypermobile feet?
Perhaps unsurprisingly to many of us, research shows that people with generalized joint hypermobility had even better outcomes with balance training than less hypermobile groups! One study found improvements in sprain recurrence, balance control, and muscle strength. Balance is a key tenet in my Integral Movement Method—the act of walking is, in fact, a balancing act.
Do I need custom orthotics?
Custom orthotics and proper footwear can go a long way in improving foot pain. While research demonstrates significant benefits, whether you specifically need them depends on your individual foot structure, symptom severity, activity level, and movement patterns. Not everyone with hypermobile feet requires orthotics—some people achieve excellent results with strengthening and movement therapy alone. An EDS-aware podiatrist can assess your feet and determine if custom orthotics would support your specific needs.
Can orthotics help with fatigue?
One study assessed the use of custom orthotics in people with EDS and found wearing custom insoles for 3 months (7 hours a day) led to improvements in foot pain, foot functionality, fatigue(!), and mental-health-related quality of life. This was an often-overlooked benefit of the research. Orthotics also help improve proprioception, ankle stability, and issues further up the kinetic chain by changing foot kinematics (or motion of the foot).
Updated January 2026
Literature Review/Research by Catherine Nation, MS, PhD
Works Cited
- Roberts & Hakim (2024). Chapter 75: Painful heels, and tired and clumsy feet Poor biomechanics in the feet causing localized pain, poor gait, and fatigue when walking. Symptomatic Editors: Clair A. Francomano, Alan J. Hakim,
- Lansdale et al. (2020). Gait biomechanics in joint hypermobility syndrome: a spatiotemporal, kinematic and kinetic analysis. Musculoskeletal Care.
- Hou et al. (2023). Balance training benefits chronic ankle instability with generalized joint hypermobility: a prospective cohort study. BMC Musculoskeletal Disorders.
- Cutts, et al. (2012) Plantar Fasciitis. Annals of The Royal College of Surgeons England.
- Petraglia, et al (2017). Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review. Muscles Ligaments and Tendons Journal.
- Berglund et al. (2005). Foot pain and disability in individuals with Ehlers – Danlos syndrome (EDS): Impact on daily life activities. Disability and Rehabilitation.
- Cimolin et al. (2014). Foot type analysis based on electronic pedobarography data in individuals with Joint Hypermobility Syndrome/ Ehlers-Danlos Syndrome Hypermobility type during upright standing. Journal of the American Podiatric Medical Association.
- Vermeulen et al. (2022) Altered multi-segment ankle and foot kinematics during gait in patients with Hypermobile Ehlers-Danlos Syndrome/Hypermobility spectrum disorder. A case-control study. Arthritis Care Research.
- Igharo et al. (2022) Skin biopsy reveals generalized small fibre neuropathy in hypermobile Ehlers–Danlos syndrome. European Journal of Neurology.
- Robbins et al. (2019) Neuromuscular Activation Differences During Gait in Patients With Ehlers-Danlos Syndrome and Healthy Adults. Arthritis Care and Research.
- Reina-Bueno et al. (2020). Custom-Made Foot Orthoses Reduce Pain and Fatigue in Patients with Ehlers-Danlos Syndrome. A Pilot Study. International Journal of Environmental Research and Public Health.


11 Comments
Lynn Moinazad - 12th August 2024
My daughter now 15 yrs was diagnosed with fibrous bar coalitions in both feet age 9, she should have had the operation last month but had to cancel due to her being very unwell since January. Just diagnosed with dysautonomia and awaiting a rheumatologist appt re EDS. I’ve been saying for over 6 years she has EDS. Is fibrous coalitions seen in EDS patients?
Jeannie Di Bon - 20th August 2024
Sorry to hear about your daughter. It is not something I am aware of or come across but be good to ask the doctor.
Deborah - 18th July 2024
I have Been dealing wih this since I was 3 years old -partly what you have said make sence. But Doctor’s are not trained to stop Ehlers Danlos if anything they get 30 to 45 minutes over the years of becoming a Doctor – I think Now we are in the 2024 more are starting to realise its a condition. Some of us don’t just sprain ankle we dislocate them as well – Now because of we are gentically we can part dislocate or fully dislocate neither is helpful. – Physios are only just training to understand Eds . a level 3 maybe 4 might know of it – If you are unsure have for a level 5 plus – if that not do able ask how much they know what the condition before they touch you – because however well meaning they can be they can cause damage by not understanding how our joints differ to someone who doesn’t have the condition – and most Pyhsio are trained in that part only – If they use the word no pain no gain stop and stop the session you have wth them . Has they have no idea about the pain level we have. So it or well type up what seem to be text book way of dealing with a joint that is misbehaving it is far more complex that what is write above – If under sure ask or seek medical advice – they are some good points made but we don’t fit in a box everyone of us is different
Jeannie Di Bon - 25th July 2024
Thank you for taking the time to comment. I totally agree – there is a lack of medical training and understanding. I hope my blogs help to fill some of that gap. And yes, everyone is individual and in an ideal world, would receive individualised care. We are working on that too.
Ann - 11th June 2023
My daughter has the exact same problem as this. We have seen multiple physios and podiatrists, all to no avail. It seems s very confusing. The pain has been for 5 years or so.
Jeannie Di Bon - 20th June 2023
Sorry to hear. Hope this was useful info.
Amy Barrick - 15th November 2022
What would it indicate if the pain is better in the morning and worsens through the day? The main pain is in the forward part of the underside of my heel, toward the arch, right as the heel is ending. And it’s awful:( I can find nothing that alleviates it. Standing is worse than walking, but waking is still pretty bad.
Jeannie Di Bon - 17th November 2022
Sorry to hear. It is very difficult to give a specific answer without seeing you walking or moving. It could be a number of things. Please do see a physiotherapist for a diagnosis. Hope it settles soon,
Jeannie
Annette - 9th November 2022
Not going barefoot in my home keeps my plantar fasciitis at bay. I wear my Birkenstocks in the house. I used to be the person who didn’t allow shoes inside. If I get lazy about it I can feel the pain start back up.
Kristyanne Robinson - 3rd July 2022
I have Eds and have dealt with plantar faciitis for years. I initially treated it in the ways you recommended above with little to no relief. I eventually encountered a sports medicine dr who told me that with eds I should not be stretching “ever” as I am never actually stretching the muscle but rather the connective tissue and therefore worsening the problem. I recently encountered a physiotherapist who was telling my daughter (also eds) to stretch for her feet and when I explained what that dr had told me she seemed quite confused. So now I’m confused. To stretch or not to stretch!? Going off my experience, at least with feet it has not been helpful. But then neither has chiro, acupuncture, massage, light therapy, heat, ice, rest, tens therapy, and a reconditioning program!
Jeannie Di Bon - 5th July 2022
Thank you for taking the time to comment. It can be a really frustrating condition. It is often caused by tight calf muscles that pull on the plantar fascia so mobilising and improving foot and lower limb function will help. I don’t recommend static stretching but do encourage dynamic stretching – where you don’t hold the stretch end of range but move in and out of a stretch. Much more beneficial.