Estimated reading time: 7 minutesHave you been told to exercise to help manage your EDS or HSD? Perhaps you have been given no instruction on how to exercise with this condition. Or perhaps you’ve been told to just do pilates or go swimming. Or maybe you’ve been sent to a physical therapist who doesn’t understand hypermobility and makes things worse?
We all have dreams – it may be to be able to garden or play pain-free with our children. Or to sit at a desk for work without neck pain. I encourage everyone to hold that dream. With appropriate, regular exercise and movement education, you never know what’s possible.
In my role as a movement therapist, I have the privilege of speaking to many people every day, living and learning to thrive despite having EDS, hypermobility, or chronic pain. We do have to make changes, but it’s not the end of the road. We just have to do things differently from before – we’ll talk about that in this blog.
There are great EDS/HSD-aware physical therapists and physiotherapists out there, but not enough!
I am working closely with The Ehlers-Danlos Society on the EDS ECHO programs to train more physical therapists in the Integral Movement Method so that we can help more EDS patients with appropriate exercise guidance. Exercise can be a source of fear or anxiety for many of us, but it does not have to be!
If we have been inactive for a while we may not be able to start right back up with the activities we once loved, but we can start somewhere.
Safe exercise practices
A mistake that is so often made in prescribing exercise programs to hypermobile patients is jumping straight in with stability and strength work. With someone just starting, this can lead to the risk of overuse injury and strain. This, in turn, can create frustration and self-blame. We may assume that there must be something wrong with us or we are doing something wrong to cause injury.
The boom-and-bust cycle can be harmful and discouraging.
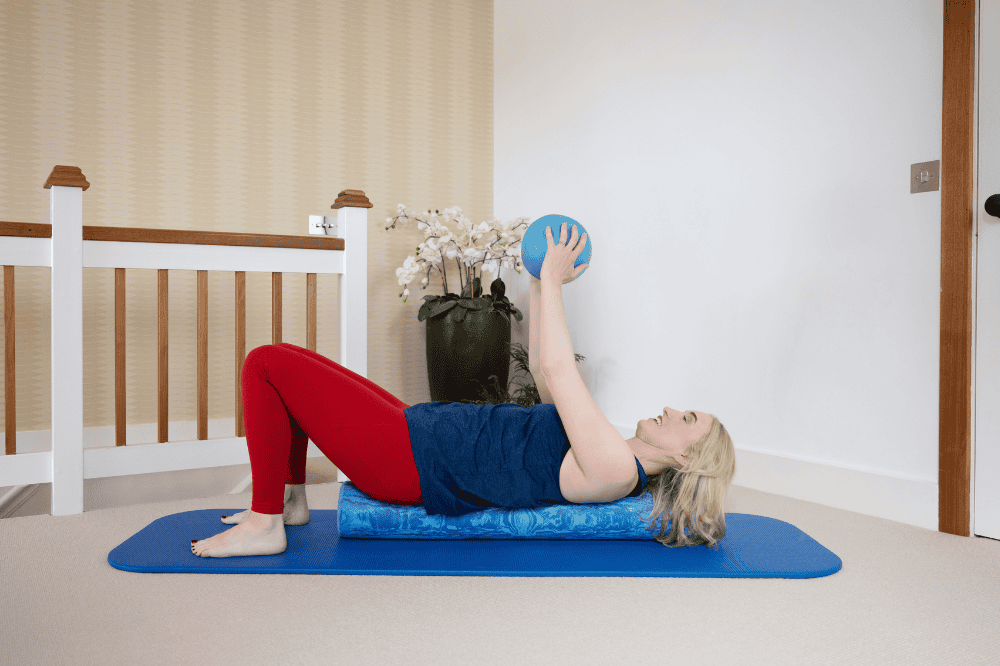
I find we need to take some steps prior to getting to the strength and stability stage and that begins with breath and relaxation. The IMM is the first evidence-based method that brings a cohesive strategy together of how to progress a hypermobile patient safely starting with fundamental principles before we even think about stability work.
In one study on people with hEDS/HSD, participants were asked about the barriers they face with exercise. 87% reported pain, 79% reported fatigue, and 50% reported that a fear of injury prevented them from exercising (1). I think these should all be taken into account when approaching exercise.
Finding your baseline with EDS exercise
I highly recommend we first find our baseline – what can we do safely without causing a flare-up? Once we find a baseline we can build up from there. This reduces, or ideally eliminates, the boom-and-bust cycle. It does not matter if that baseline is low.
I often say to my clients and The Zebra Club members that we “start low, and go slow”. This is where we can find safety with movement and exercise.
Slow progression with strengthening can also allow us to avoid irritating joints, fascia, and surrounding tissues – it is thought that our muscles activate differently than the non-hypermobile population (2). This slow and steady progression can also prevent injuries from overuse and inflammatory responses (2).
I think it is important we do not compare ourselves to others or our ‘old’ selves. For sure, there will be a period of adjustment and acceptance. I find that once we find this mentality shift of not pushing and also still moving, things begin to improve. Focusing on one baby step at a time can take you a long way.

Benefits of exercise for hypermobility
It has been reported that when people with Ehlers-Danlos syndrome experience deconditioning, this can lead to more joint laxity which leads to more weakness, instability, and more pain – which continues as a cycle (3,4).
We can break this cycle when we find a way to get back into movement and exercise without increasing pain. In fact – there are many ways that exercise or movement can help improve our quality of life beyond pain.
- Improve proprioception: Proprioception is the awareness of where we are in space. This is impaired in people with EDS (5). Multiple studies have shown we can improve proprioception with targeted exercises in EDS (4).
- Improve balance: Balance can also be improved with targeted exercise (4)
- Reduce pain: Multiple studies have shown that exercise and rehab programs can help improve pain (4). I believe the approach to movement and the role of the nervous system in pain may be important in the success of exercise on pain relief.
- Upregulation of the central nervous system is also implicated in our pain response (3). The Zebra Club scientific advisor Dr. Leslie Russek explains that small, slow, mid-range gentle movements can decrease sensitization.
- Improve stability: Maintaining muscle strength can reinforce joint stability (as well as reduce chronic widespread joint pain) (2)
- Better sleep: It has been suggested that exercise during the day is part of a sleep hygiene plan to promote better sleep, and may encourage wakefulness (6)
- Less fatigue: Muscle strengthening can decrease fatigue (2) – if we are more stable we use less energy in bracing to stabilize.
- Improve POTS and other forms of dysautonomia: Emily Rich, OT explains how in this blog post.
When working with ME/CFS, fatigue will be a factor. We need to find a way to gently increase activity and conditioning without inducing post-exertional malaise (PEM). We have a subgroup in The Zebra Club for people with energy-limiting conditions like ME/CFS and many of our members learn to move and improve pain with our classes.
Exercises to avoid with EDS
On my podcast, Finding Your Range, I’ve interviewed several people with EDS who use exercise to help manage their condition. It is essential for their mental and physical health. I’ve met climbers who live for the climbing wall, dancers who are guided by the music, and bodyboarders who cannot wait to get out on the sea.
A member of The Zebra Club online recently returned to figure skating after diligently completing my online videos three times a week for three years. That’s a commitment to a dream.
I find that when we start with breath and relaxation, and progress to proprioception, stability, balance, and posture – we find we can begin to do the things we once loved. When we have stability and control of our joints we can safely do exercise or sports that once might not have been as safe for us.
I’m never one to tell someone they should stop doing something they love. I believe there is always a way forward, even if we need to approach it differently. I’m not saying this would be easy – it requires determination, strength, commitment, and belief. I do believe that it does not matter where your starting point is today, there is always a way forward no matter how small the steps.
It’s often not the exercise that’s wrong but the approach to exercise that is wrong. We do need to work differently. I recently heard an EDS patient being told by a health professional they need to work harder than everyone else to achieve their dreams. It’s not harder – that is going to cause more stress and tension. It’s different, it’s smarter, it’s informed, and it’s safe.
It’s all about balance – rest when you need to
In my experience, yes kinesiophobia or fear of movement may lead to deconditioning. Sometimes, however, we can push too hard and our bodies MAKE us stop.
“Some people may avoid all physical exercise to prevent pain and fatigue, but this will promote physical deconditioning. Other people may persist in exercising despite pain and fatigue and stop only when pain or fatigue is extreme. However, this may over time result in dramatically reduced physical activity (7).”
As a recovering perfectionist (as I know many of us are), I have had to learn how to rest – and “rest proactively” a concept one of our lovely The Zebra Club members introduced me to. It doesn’t work when we push our bodies too far.
Pacing and working within our energy windows is crucial when managing these conditions. This can help us manage, fatigue and pain and hopefully prevent crashing.
We have presentations in the resource center in The Zebra Club app from Occupation Therapist Jo Southall and Exercise Physiologist Emily Cochrane that dive deep into pacing strategies that are useful when managing hEDS/HSD and co.
Criteria for choosing the best exercises for Ehlers-Danlos
When evaluating whether an exercise program or type of exercise is right for me, here are some things I would ask myself
- Is it increasing pain? Being a little sore after doing an exercise is to be expected, but a big increase in pain is not.
- Am I being pushed past what feels safe for me? A good physio or movement professional will help you feel comfortable and listen to you. This is a non-negotiable for me.
- Can I do it with control and not hang off of my joints or hyperextend without control?
- Do I enjoy it? If I enjoy it, I’m more likely to create a habit and continue doing it.
- Is my breath being compromised by what I’m being asked to do? I always say you should be able to have a comfortable conversation with the person next to you while exercising safely with hypermobility. If you are breath-holding, that could cause more tension in the body.
- Am I progressing at a pace that suits my body? Everyone is different – there is not one set of rules to follow. It may not be a linear progression – we often have a couple of steps back and forth. That is OK too.
- Importantly – does it make sense? I believe in educating my clients and Zebra Club members on the why. Why we are doing something, why something might be going wrong. Find an exercise professional who is happy to take the time to explain the rationale to you. Handing out a list of generic exercises that also get given to non-hypermobile patients probably isn’t the best way forward.
Here is a brief video on the “Less is more” approach to exercise:
FAQ
What is the best exercise for EDS?
There isn’t one form of best exercise for EDS. It depends on the individual and finding something you enjoy and makes you feel good. Pilates is often recommended as a safe form of exercise for building stability.
Should people with EDS lift weights?
People with EDS can lift weights. But if you decide to do this, it is vitally important you understand how to load the body safely and ensure correct alignment to avoid injury. With weights, we have to be really sure we can resist gravity. It may be something to work up to.
What exercises should people with EDS avoid?
Generally, the advice is for people with EDS to avoid contact sports like rugby, and American football. Also, high-impact sports involving jumping could be damaging to some people’s joints.
Literature review and research by Catherine Nation, MSc, PhD
Works Cited
- Simmonds et al. (2019) Exercise beliefs and behaviours of individuals with Joint Hypermobility syndrome/Ehlers–Danlos syndrome – hypermobility type. Disability and Rehabilitation.
- Russek et al. (2019) Recognizing and Effectively Managing Hypermobility-Related Conditions. Physical Therapy.
- Scheper et al. (2015) Chronic pain in hypermobility syndrome and Ehlers–Danlos syndrome (hypermobility type): it is a challenge. Journal of Pain Research.
- Buryk-Iggers et al. (2022) Exercise and Rehabilitation in People With Ehlers-Danlos Syndrome: A Systematic Review. Archives of Rehabilitation Research and Clinical Translation.
- Clayton et al. (2015). Proprioceptive precision is impaired in Ehlers–Danlos syndrome. SpringerPlus.
- Hakim et al. (2017) Chronic Fatigue in Ehlers–Danlos Syndrome—Hypermobile Type. American Journal of Medical Genetics Part C (Seminars in Medical Genetics).
- Geenen & Lumley (2018) Chapter 20: Stretched beyond the limit: Well-being and functioning in patients with Ehlers-Danlos syndrome and other hypermobility syndromes. Jacobs, J.W.G., Cornelissens, L.J.M., Veenhuizen, M.C., Hamel, B.C.J. (eds.), Ehlers Danlos syndrome, pp. 281 – 295


7 Comments
Sonja Bouma - 21st April 2025
As an EDS patient, I started rowing in 2019. I couldn’t get into the boat without help, my propriocepsus was totally confused, I learned that my coordination and balance were far off…….. But I enjoyed being on the water soooooo much, that I continued doing it. I never could have guessed that I even would row in a ‘skiff’ (single boat without a keel)! But with a lot of time, energy and struggles (and tipping over….) I CAN DO IT!!!
I might row competitions, but I the Paralympic team, there are no persons with EDS. (Amputees, blind, partly paralysed are the common groups).
I hope to find some other people with EDS who also row. I live in Zwolle (Netherlands) and I’m 50 years and getting stronger every day. I really recommend everyone to row
Jeannie Di Bon - 23rd April 2025
Thank you for sharing your experience and your perseverance to do something you love.
Michele Mathieu - 6th April 2022
I am very interested in learning more about safe exercises for people with EDS. I am 59 years old and only now learning I have EDS. All my past issues now make a great deal of sense, and in particular childhood illnesses I still have issue with today. I have always been active but osteoarthritis has set in, particularly in my knees, hips, lower back and shoulders, Seems every year a new joint becomes problematic, recently my thumps and wrists as well as some gastrointestinal issues which is why I was tested for EDS. I have what people are calling flare ups and I am getting more and more as I age. They are debilitating and I am sore everywhere, tired, lack appetite, and think I am even running a slight fever. Truly horrible. The most recent event happened during a house move. Carrying boxes and such back and forth and up and down stairs (definitely hurt) for only an hour ended up in a very painful event. My family thinks I am just a frail person these days.
I like to exercise as it makes me feel good mentally, but I pay physically. I want to know how to exercise and still care for myself and this EDS. I am seeing a physiotherapist right now and they are doing laser therapy on my left knee, helps very minimally and think I am wasting my money. They tell me to so strengthening exercises but seem to know little about my condition. I ask for exercise options but I don’t feel I am getting good advice and don’t know where to turn, No one, including me, really understands this disease which doesn’t help.
Anything you have will help immensely.
Thank you for posting.
Jeannie Di Bon - 7th April 2022
Thank you for sharing your story. I would start looking at my YouTube channel that has a wide range of exercise classes for EDS and hypermobility. You may also want to consider our community membership app – The Zebra Club. You can find out more at http://www.thezebra.club. Hope these are useful.
AlexaFaie - 11th March 2022
What do you do when you baseline is subluxations without much movement at all? I can be sitting mostly still, then maybe turn my head slightly or breathe in a little more deeply than normal, or just laugh at something funny and that’s enough to cause a subluxation or even dislocation of something somewhere in my body. And its a coin toss as to whether it will be one of the joint pops that’s mostly pain free or if its one which leads to pain. Like just now I moved my right arm to move the blanket off my lap so I could then stand up, but just moving the blanket I’ve done something to my shoulder blade area. I got a shoulder pop & now it hurts to move/turn and something feels out of place.
Is there really much hope when its this level? Like if I wake up having dislocated something in my sleep, how am I meant to be able to get to the point of trying exercises? I desperately want to be able to work on strengthening stuff but how do I start from this super low level where a simple breath can cause an issue that requires bed rest to recover from? I don’t even care about exercise in terms of activities, I’d just like to be able to move around my house without stuff falling apart.
Amber Buscemi - 4th June 2024
I was the same when I joined The Zebra Club.,I needed to start very slowly and work on alignment first, and then I could start to stabilize with very gentle exercises like the isometrics Jeannie mentioned. I’m 52 and have been at it for nearly 3 years now. I no longer have subluxations, I walk 1-2 miles per day, and I do lots of gentle and moderate level classes in TZC to keep myself from stiffening up and deconditioning. It’s a great place to start. Good luck 🦓 💪
Jeannie Di Bon - 15th March 2022
Thank you for sharing your story. Sorry to hear you are struggling with subluxations. Have you managed to see an EDS aware physio to help give you some tactile feedback and guidance?
It is hard for me to give specific advice as I do not know your medical history or how you move. But it sounds like alignment is needed together with some isometric work first to get the joint working. Again, ideally this would be done with some assistance from a physio or movement professional to help you ensure alignment is correct.