
Estimated reading time: 7 minutesHeadaches are a frequent complaint among my hypermobile clients and The Zebra Club community.
I’ve suffered headaches & migraines for as long as I can remember. I must have had headaches at a young age because I have a vague memory of asking for orange flavoured aspirin from my mum.
But the real issues started when the migraines began when I was 19 and just started work in an office.
They happened every day and came with an aura, nausea, and sickness. They always arrived with my menstrual cycle, tiredness, or stress.
I’ve learnt to manage them with movement, meditation, cranial sacral therapy, and medication. Being post menopausal now, I think they are slowing down, but I have sympathy with anyone who lives with this condition.
Let’s learn more about headaches in general.
Headaches are a common problem in EDS and hypermobility
Headache has been characterized as “one of the most common and disabling types of pain in hEDS (1). It is often the first presenting symptom and cause of disability in EDS/HSD (2).
In a recent study of people with either hEDS/HSD or another form of EDS, 66% had head and neck problems, including headaches, neck pain, facial pain, neck instability, or a combination of these (3).
Another report estimated migraines occur in somewhere between 40% and 75% of people with hypermobility. That is huge compared to the general population, where the prevalence is estimated to be about 14% (2).
So it’s clear that if you are experiencing headaches, not only are you not alone, but you are with the majority of hypermobile individuals.
There are a number of causes of headaches and migraines in EDS
Headaches seem to vary from a frequent occurrence to chronic and debilitating. Headaches in EDS can be linked to a wide range of conditions. However, exactly why EDS is related to these is not always understood. Some of these conditions include (1-4):
- Migraine
- Idiopathic Intracranial Hypotension (increased pressure of cerebrospinal fluid)
- Chiari malformation – spinal cord and brain compression
- Upper Cervical Instability
- Dysautonomia – Such as Orthostatic Hypotension (OH) or Postural Orthostatic Tachycardia Syndrome (POTS)
- Temporomandibular Joint Disorders (TMJD)
- Muscle tension (Tension Type Headache)
- Cervicogenic headaches from other neck issues, like Occipital Neuralgia
- Medication overuse headache
Anecdotally, we could probably add sleep issues, menopause, and mast cell activation syndrome (MCAS) as common issues that likely contribute to headaches.
Migraines and hypermobility
The recent National Health Service guidelines on migraine management report that migraines may be responsible for many more symptoms than simply a headache. It is considered an invisible and common disability for many people.
These non-headache symptoms can include fatigue, coat hanger pain, dizziness, poor quality sleep, and brain fog. These are also all symptoms often reported by people with EDS or HSD.
A migraine is more than a headache. This condition is characterized by frequent moderate to severe attacks that last 4 -72 hours. They are often one-sided, pulsating, and can be associated with nausea, light and noise sensitivity, and can be disabling (4). Migraines, like hypermobility, are more common in women (4).
A migraine is considered chronic if there are attacks for 15 or more days a month, for more than 3 months, with “migranous features” for 8 days a month or more (2)
It was not surprising to learn that migraine was found to be 3 times more likely to occur in patients with joint hypermobility syndrome (5).
Migraines in hypermobile people were found to actually be more severe than in non-hypermobile patients. They occurred more frequently, had more severe symptoms, were more at risk for having chronic migraines, and were usually not adequately treated (5).
Management of migraine may require a multistep approach addressing lifestyle factors (like avoiding triggers), medication, and neuromodulation (2). If you have chronic migraine, it may be helpful to see a neurologist, as newer medications like calcitonin gene-related peptide (CGRP) inhibitors could be helpful (2).

A note on vestibular migraines
I have a handful of clients who experience another type of migraine called vestibular migraines that complicate the headache picture even more. This type of migraine is often characterized as migraines with vertigo.
The vestibular system’s job is to detect where the head is in space and how it is moving. This is done through nerve signals between the vestibular system in the inner ear and the brain. Vestibular migraine is also rare, affecting up to 2.7% of the general population (6). However, we could find no numbers for its prevalence in hEDS/HSD specifically.
Officially, diagnostic criteria include having episodes of moderate to severe vestibular symptoms lasting 5 minutes to 72 hours, with a history of migraines, and having one of these symptoms with 50% of the vestibular episodes: one-sided, pulsating headache; light or sound sensitivity; and/or aura. Additionally, other reasons for having vestibular symptoms have been ruled out (6).
Some examples of vestibular symptoms include (6):
- Internal vertigo (sensation that body is in motion)
- External vertigo (sensation that the room is spinning)
- Positional vertigo with changes in head position
- Visually induced vertigo
- Vertigo with head motion
- Head motion-induced dizziness with nausea
Vestibular migraines, like other migraines, are more common in women. They also seem to have an autosomal dominant inheritance pattern similar to that seen in hEDS, meaning a child of a parent has a 50% chance of inheriting the condition (7).
It was also interesting to learn that in postmenopausal people, typical migraines are sometimes replaced by episodes of vertigo, dizziness, or feeling off balance (7).
This type of migraine may need to be treated by a vestibular migraine experienced specialist or a Neuro-otologist, sometimes an otolaryngologist (ENT). Vestibular Rehab with a specialised physical therapist may also help.
Investigating the link between upper cervical instability, hEDS/HSD, and headaches
In 2023, the scientific advisor to The Zebra Club, Dr. Leslie Russek, published the first expert consensus and recommendations for screening for and managing Upper Cervical Instability (UCI).
This was done along with an international team of physical /physiotherapy clinicians and researchers, and a hypermobility specialist rheumatologist.
They state that mild UCI is relatively common among people with hEDS/HSD, impacting between 52-66% of people. However, severe UCI is thought to be uncommon, impacting only 5% of people with hEDS/HSD (8).
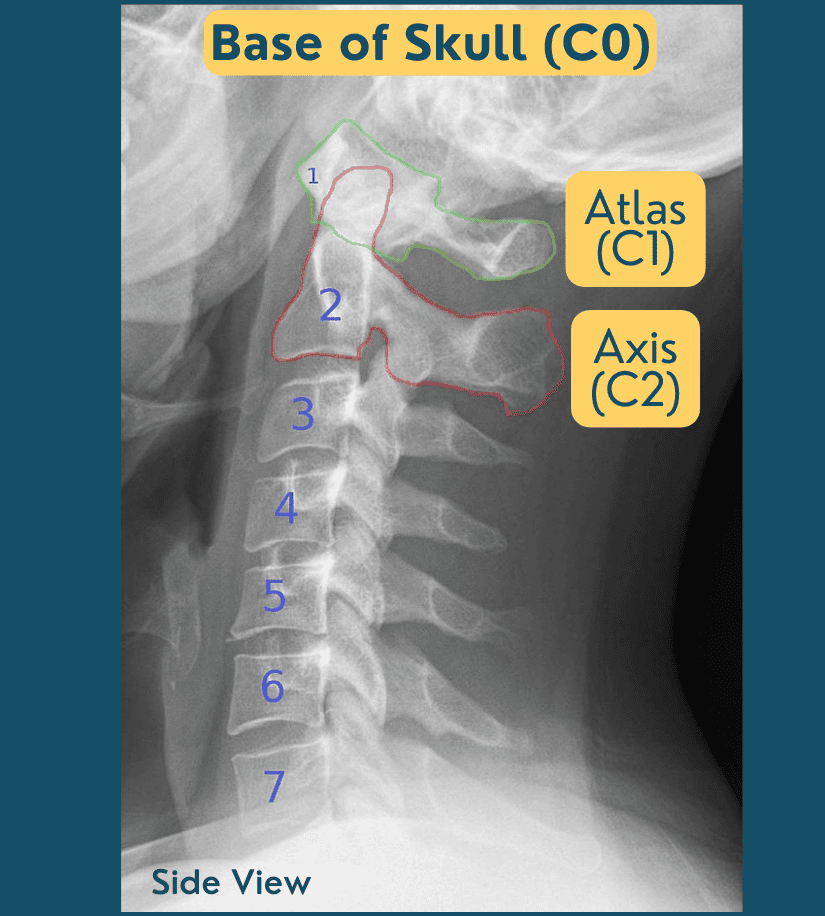
Craniocervical instability (CCI) is ligament laxity in the joint between the atlas (Cranial vertebra 1 or C1) and the occiput or base of the skull (C0). There can also be instability in the atlas (C1) and the axis (C2); this is called atlantoaxial stability (AAI). Together, these can be called Upper Cervical Instability (UCI).
Symptoms of UCI exist on a spectrum and can include headaches, neck or facial pain, dizziness, vertigo, nausea, numbness/tingling, shortness of breath, difficulty speaking, vision changes (blurred, tunnel vision, auras), hearing changes, difficulty swallowing, choking, sleep apnea, memory deficits, pre-syncopal episodes (feeling like you’re going to faint) (8).
Determination Criteria for Upper Cervical Instability
Russek et al. classify patients as having low, moderate, or high “irritability.” This is a measure of mechanical irritability, or increased symptoms with movement. This is based on how severe the condition is, how easily it is flared, and how long it takes for symptoms to calm down after being flared.
Importantly, this may change from day to day and progress towards lower irritability as patients improve. These are important to keep in mind when looking at recommended interventions.
Three criteria must be met for UCI:
- Symptoms are consistent with musculoskeletal and/or neurological UCI.
- Symptoms are altered by neck movement or position.
- For example: Increased symptoms when leaning forward or looking down
- Increased symptoms with neck motions like flexing, extending, or rotating
- Mechanical irritability with a physical exam
Useful assessment tools are provided for use by physical/physiotherapists as well as recommendations for when to make referrals. I don’t recommend making this determination yourself.
Exploring self-treatment for neck-related headache issues
Importantly, some strategies can help with UCI. The authors recommended numerous interventions organized by levels of irritability. Russek et al. provide several very helpful intervention suggestions to help with UCI symptoms.
Many of these strategies are things I have already found useful with my clients, and strategies I made sure were included in The Zebra Club App
- Sitting, standing, and sleep posture, positioning, and body support
- Body awareness and mindfulness in various positions (sitting, standing, lying down).
- The Zebra Club app has classes specifically for headaches and coathanger pain.
- Relaxation and autonomic nervous system balancing (not requiring neck movement).
- The Head, Neck, and Shoulders Meditation Audio in The Zebra Club is reportedly very helpful for headache pain management.
- Breathing (diaphragmatic or slow breathing)
- Try one of the breathing classes in The Zebra Club, or this one
- Education in pain neuroscience
- Mindful use of language to enhance feelings of safety
- Self-care “toolbox”
- pain management strategies like TENS, topicals, relaxation, etc.
Members of The Zebra Club can learn more about Upper Cervical Instability in the Resources section. We have presentations by Dr. Leslie Russek (2023) and Dr. Ann McCarthy (2025), who were both authors on the Upper Cervical Instability Guidelines paper. We are also being joined for a presentation by Dr. Munro, a migraine specialist in July, 2025.
In this video, I discuss more about my experience working with clients who have neck pain and headaches. I then teach a movement class. Please note – these exercises may not be suitable for everyone.
They should not cause increased pain or neurological symptoms. Please seek medical advice if they do. They are not designed to replace any medical guidance you have been given. If you are highly irritable in the neck, please work one-on-one with a physical therapist.
FAQ
Does hypermobility give you headaches?
Headaches are common in hypermobility and can be the result of many things like migraine, upper cervical instability, dysautonomia, TMJ disorder, muscle tension, and other neck issues. In fact, headaches are characterized as one of the most common and disabling pains in hypermobility.
How to get rid of EDS headaches?
There are things we can do to address some causes of EDS headaches, like addressing posture, strength, tension, and nervous system regulation. It is advisable to seek medical care from an EDS aware neurologist or primary care, especially is something is new, different, or profound.
What does EDS do to the brain?
EDS primarily impacts the body’s connective tissues but it can impact the brain and nervous system in a broader way. Issues like blood flow to the brain, cerebrospinal fluid flow issues and leaks, and autonomic function. Structually there could be issues of Chiari Malformation where the brain tissue extends into the spinal canal. Some people with EDS may experience intracranial hypertension too where there is increased pressure in the skull.
Are headaches common in EDS?
Headaches are very common in EDS. It is one of the most frequently reported and disabling symptoms and can occur for a variety of different reasons, like migraine, craniocervical instability, dysautonomia, TMJ disorder, muscle tension, and other neck issues.
Updated for 2025
Literature review by Catherine Nation, MSC, PhD
Works Cited
- Levy et al. (2020) An investigation of headaches in Hypermobile Ehlers-Danlos Syndrome. Annals of Psychiatry and Clinical Neuroscience.
- Mehta et al (2024) Headache disorders in patients with Ehlers-Danlos syndromes and hypermobility spectrum disorders. Frontiers in Neurology.
- Malhotra et al. (2020) Headaches in hypermobility syndromes: A pain in the neck? PMID: 32940405
- Henderson et al. (2017) Neurological and Spinal Manifestations of the Ehlers-Danlos Syndromes PMID: 28220607
- Puledda et al. (2015) A study of migraine characteristics in joint hypermobility syndrome a.k.a. Ehlers-Danlos syndrome, hypermobility type.
- Lempert et al. (2022) Vestibular Migraine: Diagnostic criteria (Update).
- Stolte et al. (2015) Vestibular Migraine. PMID: 24847169
- Russek et al. (2023) Presentation and physical therapy management of upper cervical instability in patients with symptomatic generalized joint hypermobility: International expert consensus recommendations.


8 Comments
Johanna - 13th December 2025
Thanks for this informative Video ! Do You have any Tipps in sleeping? As my Pain already accurs directly in the Morning.
Jeannie Di Bon - 16th December 2025
Yes we do – there is a blog on sleeping here too.
Sleeping with hypermobility: A comprehensive guide
Sandra Smith - 5th March 2025
Any help with headaches that only start when I’m sleeping and occur nightly
Jeannie Di Bon - 7th March 2025
It is always best to consult with a medical professionals about any new types of headaches. Hope you have someone you can see for a medical consult.
Martina Ingemarsson - 10th April 2024
This article was very helpful to me, thank you! Very pedagogical. I will now make sure to watch the YouTube episode and class.
Jeannie Di Bon - 11th April 2024
Thank you – I am so glad you enjoyed this headache article.
Kylie - 29th March 2024
My daughter often tells us she is seeing one colour could be pink, blue, red or green then after a little while states she has a headache. Just interested what category this may fall into
Jeannie Di Bon - 2nd April 2024
Thank you for taking the time to comment. I cannot give any medical advice on here but do recommend checking with your medical practitioner.